The optimization of maternal micronutrient status during pregnancy represents one of the most critical yet complex challenges in contemporary obstetric care, extending far beyond the traditional one-size-fits-all approach of standard prenatal vitamins to encompass sophisticated understanding of individual variations in metabolism, absorption, and utilization of essential nutrients. The emerging paradigm of precision nutrition recognizes that pregnant women exhibit remarkable heterogeneity in their micronutrient requirements, influenced by genetic polymorphisms, dietary patterns, environmental exposures, and underlying health conditions that collectively determine optimal supplementation strategies for each individual.
The consequences of micronutrient deficiencies during pregnancy extend across generations, affecting not only immediate maternal health and pregnancy outcomes but also programming fetal development in ways that influence lifelong health trajectories and disease susceptibility. Understanding the intricate relationships between maternal micronutrient status and fetal development requires appreciation of the dynamic interplay between nutrient availability, placental transport mechanisms, and the rapidly changing nutritional demands of growing fetal tissues during critical windows of organogenesis and growth.
Contemporary research has revealed that micronutrient deficiencies represent a global phenomenon affecting pregnant women across all socioeconomic strata and geographic regions, with deficiencies in iron, folate, vitamin D, iodine, and zinc emerging as particularly prevalent and consequential for maternal and fetal health outcomes. The traditional approach of universal supplementation with standard formulations has proven inadequate for addressing the complex nutritional needs of diverse populations, necessitating more sophisticated approaches that consider individual risk factors, bioavailability variations, and the synergistic interactions between different nutrients.
The concept of precision nutrition represents a revolutionary shift toward personalized dietary recommendations based on individual genetic, metabolic, and environmental characteristics, offering unprecedented opportunities to optimize maternal nutrition throughout pregnancy. This approach recognizes that nutrient requirements vary substantially between individuals and that optimal supplementation strategies must be tailored to address specific deficiency risks, absorption capacities, and metabolic demands that characterize each pregnant woman’s unique nutritional profile.
Pathophysiology of Micronutrient Metabolism in Pregnancy
The physiological adaptations that occur during pregnancy profoundly alter micronutrient metabolism, creating unique challenges for maintaining adequate nutritional status while supporting the extraordinary demands of fetal growth and development. Maternal blood volume expansion, which can increase by up to fifty percent during pregnancy, significantly dilutes circulating nutrient concentrations and necessitates increased intake to maintain adequate tissue levels of essential micronutrients. This hemodilution effect particularly impacts nutrients that are primarily transported bound to plasma proteins, creating apparent deficiencies that may not reflect true tissue depletion.
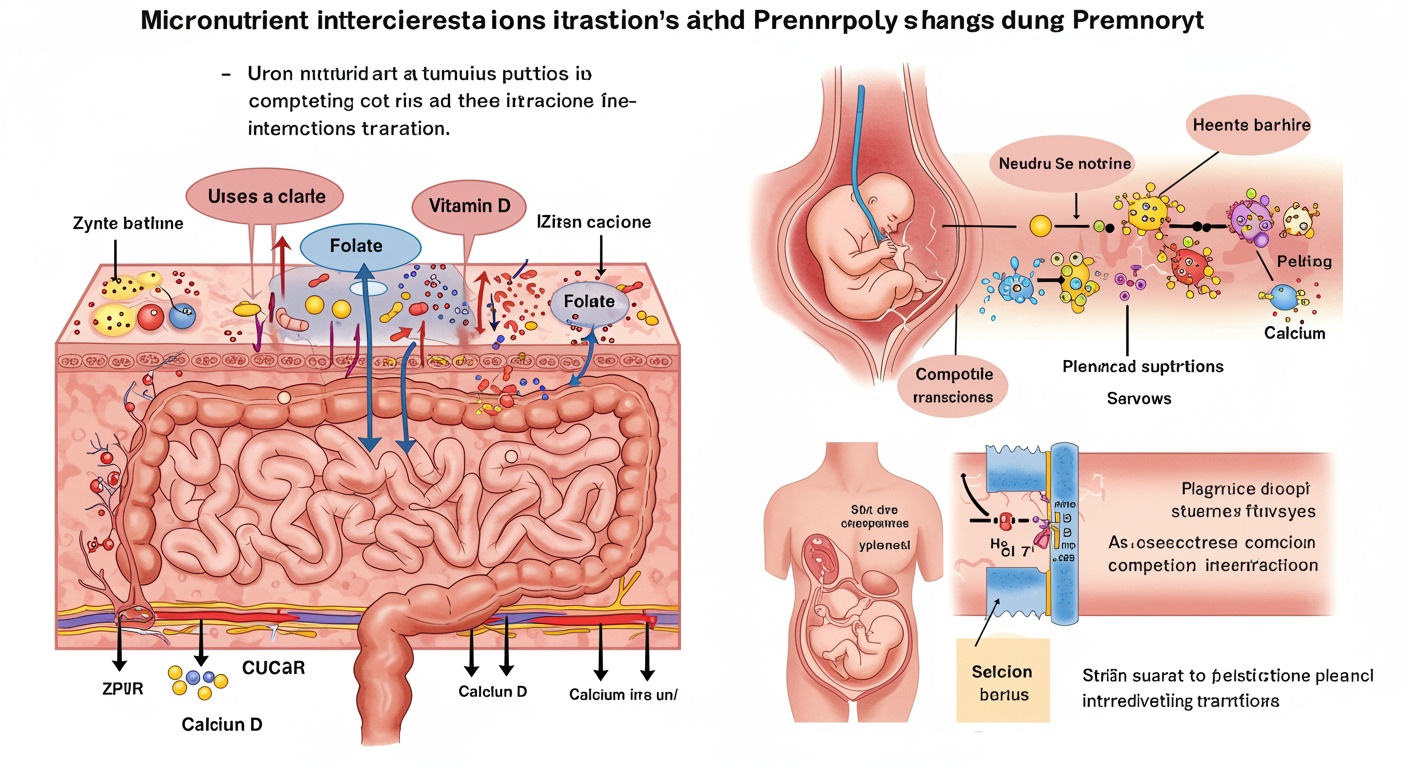
Gastrointestinal adaptations during pregnancy, including decreased gastric motility and altered pH levels, significantly influence micronutrient absorption and bioavailability, with some nutrients experiencing enhanced absorption while others face reduced uptake efficiency. The dramatic increase in progesterone levels during pregnancy relaxes smooth muscle throughout the digestive tract, prolonging transit time and potentially enhancing absorption of nutrients that require extended contact time with intestinal mucosa, while simultaneously reducing absorption of nutrients sensitive to altered gastric pH or prolonged exposure to digestive enzymes.
Placental transport mechanisms represent sophisticated biological systems that actively regulate the transfer of micronutrients from maternal circulation to the developing fetus, with different nutrients utilizing distinct transport pathways that vary in their efficiency and regulation throughout pregnancy. The placenta demonstrates remarkable selectivity in nutrient transport, actively concentrating certain micronutrients in fetal circulation while limiting the transfer of others, creating maternal-fetal gradients that can significantly deplete maternal stores while maintaining adequate fetal supply.
Renal adaptations during pregnancy, including increased glomerular filtration rate and altered tubular reabsorption, significantly impact the excretion and retention of water-soluble vitamins and minerals, often requiring increased intake to compensate for enhanced urinary losses. The increased blood flow to the kidneys during pregnancy can result in substantial losses of nutrients that are not efficiently reabsorbed, particularly affecting vitamins B6, B12, and folate, which may require supplementation levels far exceeding non-pregnant recommendations.
The metabolic demands of pregnancy create dynamic changes in micronutrient utilization patterns, with certain nutrients experiencing dramatically increased turnover rates to support protein synthesis, DNA replication, and cellular proliferation required for fetal growth and maternal tissue expansion. These increased metabolic demands are further complicated by alterations in nutrient storage and mobilization patterns, with pregnancy hormones influencing the release of stored nutrients from maternal tissues while simultaneously promoting the accumulation of certain nutrients in preparation for lactation.
Critical Micronutrients: Individual Assessment and Requirements
Iron represents perhaps the most complex and clinically significant micronutrient challenge during pregnancy, with requirements increasing dramatically from approximately eighteen milligrams per day in non-pregnant women to twenty-seven milligrams during pregnancy, reflecting the substantial demands for expanded maternal blood volume, placental development, and fetal iron stores. The assessment of iron status during pregnancy requires sophisticated understanding of the multiple biomarkers that reflect different aspects of iron metabolism, including serum ferritin, transferrin saturation, soluble transferrin receptor, and hepcidin levels, each providing unique insights into iron availability and utilization.
The pathophysiology of iron deficiency during pregnancy extends beyond simple inadequate intake to encompass complex interactions between absorption efficiency, competing dietary factors, and individual genetic variations in iron metabolism. Genetic polymorphisms in genes encoding iron transport proteins, including transferrin, ferroportin, and hepcidin, significantly influence individual iron requirements and response to supplementation, necessitating personalized approaches that consider both phenotypic markers and genetic predisposition to iron deficiency.
Iron deficiency anemia during pregnancy carries profound consequences for both maternal and fetal health, including increased risks of preterm delivery, low birth weight, and maternal mortality, while also affecting long-term cognitive and behavioral development in offspring. The timing of iron deficiency during pregnancy critically influences its impact on fetal development, with early pregnancy deficiency affecting organ development and brain growth, while later deficiency primarily impacts fetal iron stores and birth weight.
Folate metabolism during pregnancy involves complex biochemical pathways that support DNA synthesis, methylation reactions, and amino acid metabolism essential for rapid cellular proliferation and differentiation during fetal development. The most well-recognized consequence of folate deficiency involves neural tube defects, but emerging research reveals that inadequate folate status affects multiple aspects of fetal development, including cardiovascular formation, placental function, and epigenetic programming that influences lifelong health outcomes.
Individual variations in folate requirements during pregnancy are substantially influenced by genetic polymorphisms in folate metabolism enzymes, particularly methylenetetrahydrofolate reductase variants that affect the conversion of folate to its active form. Women carrying certain genetic variants may require folate supplementation levels substantially higher than standard recommendations to achieve adequate tissue levels and prevent deficiency-related complications.
Vitamin D deficiency during pregnancy has emerged as a global health concern affecting up to ninety percent of pregnant women in certain populations, with deficiency defined by serum 25-hydroxyvitamin D levels below thirty nanograms per milliliter. The consequences of vitamin D deficiency extend beyond classical calcium homeostasis to encompass immune function, inflammatory responses, and gene expression regulation that influences multiple aspects of maternal and fetal health.
The assessment of vitamin D status during pregnancy requires consideration of seasonal variations, sun exposure patterns, skin pigmentation, and dietary intake, all of which contribute to substantial individual differences in vitamin D synthesis and requirements. Geographic latitude, cultural practices regarding sun exposure, and the use of sunscreen significantly impact vitamin D production, necessitating individualized assessment and supplementation strategies based on multiple risk factors.
Iodine requirements during pregnancy increase substantially to support increased maternal thyroid hormone production and fetal thyroid development, with inadequate iodine intake leading to maternal and fetal hypothyroidism that can have irreversible effects on fetal brain development. The assessment of iodine status relies primarily on urinary iodine concentrations, which reflect recent intake but may not accurately represent long-term iodine status or thyroid function.
Advanced Diagnostic Approaches and Biomarker Assessment
The accurate assessment of micronutrient status during pregnancy requires sophisticated diagnostic approaches that extend beyond traditional single-biomarker measurements to encompass comprehensive evaluation of nutrient stores, functional markers, and metabolic indicators that provide insights into tissue-level nutrient adequacy. Contemporary diagnostic strategies recognize that standard reference ranges developed in non-pregnant populations may not accurately reflect optimal nutrient status during pregnancy, necessitating pregnancy-specific reference values that account for physiological adaptations and increased nutritional demands.
Functional biomarkers represent powerful tools for assessing micronutrient adequacy by measuring the activity of nutrient-dependent enzymes or the concentration of metabolites that reflect tissue-level nutrient status. For iron assessment, the measurement of zinc protoporphyrin provides insights into functional iron deficiency at the cellular level, while transferrin receptor measurements reflect tissue iron demands independent of inflammatory status that can confound interpretation of traditional iron markers.
The emerging field of metabolomics offers unprecedented opportunities to assess micronutrient status through comprehensive analysis of metabolite profiles that reflect the integrated effects of nutrient availability on cellular metabolism. Metabolomic approaches can identify subtle changes in nutrient-dependent metabolic pathways before clinical deficiency symptoms develop, enabling early intervention to prevent adverse outcomes.
Genetic testing for polymorphisms affecting micronutrient metabolism provides valuable information for individualizing supplementation strategies, particularly for nutrients like folate, vitamin B12, and vitamin D, where genetic variations significantly influence requirements and response to supplementation. The integration of genetic information with traditional biomarker assessment enables more precise determination of individual nutrient needs and optimal supplementation approaches.
Point-of-care testing technologies are increasingly available for rapid assessment of key micronutrients during routine prenatal visits, enabling immediate identification of deficiencies and prompt initiation of appropriate interventions. These technologies are particularly valuable in resource-limited settings where laboratory access may be restricted, allowing for widespread screening and treatment of micronutrient deficiencies.
The timing of micronutrient assessment throughout pregnancy requires careful consideration of the dynamic changes in nutrient metabolism and requirements that occur across different gestational periods. Early pregnancy assessment establishes baseline nutritional status and identifies pre-existing deficiencies that may impact early fetal development, while repeated assessments throughout pregnancy monitor the adequacy of supplementation and the development of new deficiencies.
Precision Nutrition: Individualized Supplementation Strategies
The implementation of precision nutrition approaches in pregnancy requires comprehensive assessment of individual risk factors, including genetic predisposition, dietary patterns, absorption capacity, and metabolic demands, to develop personalized supplementation strategies that optimize maternal and fetal outcomes while minimizing risks of excessive intake or adverse interactions. This individualized approach recognizes that optimal micronutrient status cannot be achieved through universal supplementation protocols but requires tailored interventions that address the unique characteristics and needs of each pregnant woman.
Genetic-based personalization represents a rapidly advancing area of precision nutrition, with growing understanding of how specific genetic variants influence micronutrient requirements and response to supplementation. Women carrying variants in genes affecting folate metabolism may require significantly higher folate intake to achieve adequate tissue levels and prevent neural tube defects, while variants affecting vitamin D metabolism may necessitate different supplementation strategies to maintain optimal vitamin D status.
Dietary assessment forms a crucial component of individualized supplementation strategies, with detailed evaluation of food intake patterns, cultural dietary practices, and food preferences providing insights into baseline nutrient intake and identifying specific nutrients at risk for deficiency. Advanced dietary assessment techniques, including food frequency questionnaires, dietary recalls, and emerging technologies such as dietary photography and mobile applications, enable more accurate characterization of nutrient intake patterns.
The optimization of supplement formulations represents another critical aspect of precision nutrition, with consideration of nutrient interactions, absorption enhancers and inhibitors, and individual tolerance factors that influence supplement effectiveness and acceptability. The timing of supplement administration, the chemical form of nutrients, and the presence of cofactors can significantly impact bioavailability and therapeutic effectiveness.
Individual absorption capacity varies substantially between women and can be influenced by factors including gastric pH, intestinal transit time, concurrent medications, and underlying gastrointestinal conditions that affect nutrient uptake. Women with conditions such as celiac disease, inflammatory bowel disease, or gastric bypass surgery may require specialized supplementation approaches that account for altered absorption patterns and increased nutrient losses.
The monitoring of supplementation effectiveness requires regular assessment of biomarker responses and clinical outcomes to ensure that individualized interventions achieve desired improvements in nutritional status. This monitoring approach enables real-time adjustments to supplementation protocols based on individual response patterns and changing requirements throughout pregnancy.
Nutrient Interactions and Synergistic Effects
The complex interactions between different micronutrients significantly influence their absorption, metabolism, and biological effectiveness, necessitating careful consideration of nutrient combinations and ratios in supplementation strategies. These interactions can be either synergistic, where the presence of one nutrient enhances the utilization of another, or antagonistic, where nutrients compete for absorption or interfere with each other’s metabolic functions.
Iron and vitamin C demonstrate a well-characterized synergistic relationship, with vitamin C enhancing iron absorption through reduction of ferric iron to the more readily absorbed ferrous form while also forming chelation complexes that maintain iron solubility in the alkaline environment of the small intestine. The optimal ratio of vitamin C to iron for maximizing absorption appears to be approximately four to one by weight, though individual variations in gastric acidity and other dietary factors can influence the effectiveness of this combination.
Calcium and iron exhibit competitive interactions at the level of intestinal absorption, with high calcium intake potentially reducing iron absorption through competition for shared transport mechanisms. However, the clinical significance of this interaction remains controversial, with some studies suggesting that the inhibitory effect is primarily acute and may be overcome through adaptive mechanisms with chronic supplementation.
Zinc and copper demonstrate complex interactions that can lead to deficiency of one mineral when the other is supplemented in high doses, highlighting the importance of balanced supplementation approaches that consider the interdependence of these essential trace elements. The ratio of zinc to copper in supplementation protocols should typically be maintained between eight to one and fifteen to one to prevent interference with copper absorption and metabolism.
Folate and vitamin B12 function as cofactors in overlapping metabolic pathways, particularly in one-carbon metabolism and DNA synthesis, with deficiency of either nutrient potentially masking or exacerbating the effects of deficiency in the other. The phenomenon of folate-induced masking of vitamin B12 deficiency represents a significant clinical concern, as folate supplementation can correct the hematological manifestations of vitamin B12 deficiency while allowing neurological complications to progress.
Fat-soluble vitamins A, D, E, and K compete for absorption and transport mechanisms, with excessive intake of one potentially interfering with the absorption and utilization of others. The optimal balance of fat-soluble vitamins requires consideration of individual intake patterns and the presence of conditions that affect fat absorption and metabolism.
Special Populations and Unique Considerations
Adolescent pregnancy presents unique nutritional challenges due to the competing demands of maternal growth and fetal development, requiring increased attention to micronutrient adequacy and specialized supplementation approaches that address the higher nutritional requirements of this population. Adolescent mothers face elevated risks of multiple micronutrient deficiencies due to poor dietary habits, increased physiological demands, and socioeconomic factors that may limit access to adequate nutrition.
Multiple gestations dramatically increase micronutrient requirements due to the substantially higher demands for fetal growth and development, with women carrying twins or higher-order multiples requiring significantly increased supplementation levels for most micronutrients. The assessment and management of micronutrient status in multiple pregnancies requires specialized protocols that account for the increased physiological stress and nutritional demands.
Vegetarian and vegan pregnancies require careful attention to nutrients that are primarily obtained from animal sources, including vitamin B12, iron, zinc, and omega-3 fatty acids, with specialized supplementation strategies needed to prevent deficiencies that could affect maternal and fetal health. The bioavailability of micronutrients from plant-based sources often differs significantly from animal sources, necessitating higher intake levels to achieve adequate tissue status.
Women with pre-existing medical conditions, including diabetes, gastrointestinal disorders, and autoimmune diseases, may have altered micronutrient requirements and absorption patterns that necessitate individualized assessment and supplementation approaches. Medications used to manage chronic conditions can also affect micronutrient status through effects on absorption, metabolism, or excretion.
Ethnic and genetic variations in micronutrient metabolism significantly influence optimal supplementation strategies, with certain populations demonstrating higher prevalence of genetic variants that affect nutrient requirements. For example, individuals of African descent have higher rates of lactase non-persistence, potentially affecting calcium absorption, while certain Asian populations have higher rates of variants affecting alcohol and folate metabolism.
Geographic and environmental factors, including altitude, climate, and soil mineral content, can significantly influence micronutrient requirements and availability, necessitating region-specific supplementation recommendations. Women living at high altitudes may have increased iron requirements due to physiological adaptations to reduced oxygen availability, while those in regions with selenium-deficient soils may require selenium supplementation.
Emerging Technologies and Future Directions
The integration of artificial intelligence and machine learning technologies into nutritional assessment and supplementation recommendation systems represents a promising frontier for advancing precision nutrition approaches during pregnancy. These technologies can analyze complex patterns in biomarker data, dietary intake, genetic profiles, and clinical outcomes to identify optimal supplementation strategies for individual women and predict risks of deficiency development.
Nutrigenomics research continues to reveal new insights into the genetic determinants of micronutrient requirements and response to supplementation, with ongoing studies identifying novel genetic variants that influence nutrient metabolism and optimal intake levels. The expanding understanding of genetic influences on nutrition opens possibilities for increasingly sophisticated personalized supplementation approaches based on comprehensive genetic profiling.
Novel biomarkers and diagnostic technologies are being developed to provide more accurate and comprehensive assessment of micronutrient status, including advanced metabolomic approaches that can identify subtle changes in nutrient-dependent metabolic pathways before clinical deficiency develops. These emerging diagnostic tools may enable earlier identification and intervention for micronutrient deficiencies.
Innovative supplement delivery systems, including controlled-release formulations, targeted delivery mechanisms, and personalized compounding approaches, offer opportunities to optimize bioavailability and minimize adverse effects while providing precise dosing tailored to individual requirements. These technologies may be particularly valuable for nutrients with narrow therapeutic windows or those prone to gastrointestinal side effects.
Mobile health technologies and digital therapeutics are increasingly being integrated into nutritional care during pregnancy, providing platforms for continuous monitoring of dietary intake, supplement adherence, and symptom tracking that can inform real-time adjustments to supplementation protocols. These technologies offer opportunities for more responsive and personalized nutritional care.
Research into the microbiome’s role in micronutrient metabolism is revealing new insights into how gut bacterial populations influence nutrient absorption, synthesis, and utilization, opening possibilities for microbiome-targeted interventions to optimize nutritional status during pregnancy.
Clinical Implementation and Practical Considerations
The successful implementation of precision nutrition approaches in clinical practice requires systematic integration of comprehensive assessment protocols, individualized supplementation strategies, and ongoing monitoring systems that can be feasibly incorporated into routine prenatal care. This implementation process must balance the theoretical benefits of personalized approaches with practical considerations including cost, accessibility, and provider training requirements.
Healthcare provider education represents a critical component of successful precision nutrition implementation, with practitioners requiring knowledge of advanced micronutrient assessment techniques, interpretation of genetic and biomarker data, and individualized supplementation strategies. Training programs must address both the scientific foundations of precision nutrition and practical skills for implementing personalized approaches in diverse clinical settings.
Cost-effectiveness considerations play important roles in determining the feasibility and sustainability of precision nutrition approaches, with careful analysis required to identify interventions that provide sufficient clinical benefit to justify additional costs associated with comprehensive assessment and individualized supplementation. Economic analyses should consider both short-term costs and long-term savings associated with improved maternal and fetal outcomes.
Quality assurance in supplement manufacturing and testing becomes increasingly important as supplementation strategies become more individualized and precise, with rigorous standards needed to ensure accuracy of dosing, purity of ingredients, and consistency of formulations. Regulatory frameworks may need adaptation to accommodate personalized supplementation approaches while maintaining appropriate safety standards.
Patient education and engagement strategies must be developed to help pregnant women understand the rationale for individualized supplementation approaches and maintain adherence to potentially complex supplement regimens. Educational materials should address common misconceptions about supplementation while providing clear guidance on proper use and expected benefits.
Integration with existing healthcare systems requires careful consideration of workflow modifications, electronic health record adaptations, and coordination between different healthcare providers involved in prenatal care. Successful implementation requires support from healthcare administrators and alignment with existing quality improvement initiatives.
Safety Considerations and Risk Management
The implementation of precision nutrition approaches must incorporate comprehensive safety assessment and risk management strategies to prevent adverse effects associated with individualized supplementation protocols, particularly given the potential for higher dosing levels than traditional universal supplementation approaches. Safety considerations must address both the risks of nutrient deficiency and the potential for toxicity from excessive intake.
Upper intake limits for micronutrients during pregnancy require careful consideration of both maternal and fetal safety, with recognition that pregnancy-specific safety data may be limited for certain nutrients and dosing levels. The establishment of appropriate safety margins requires integration of available toxicological data with consideration of individual variation in tolerance and metabolism.
Monitoring protocols for identifying and managing adverse effects of supplementation must be integrated into individualized nutrition programs, with clear guidelines for recognizing signs of nutrient toxicity and protocols for dose adjustment or discontinuation when indicated. Healthcare providers must be trained to recognize both common and rare adverse effects associated with micronutrient supplementation.
Drug-nutrient interactions represent important safety considerations, particularly for women taking medications for chronic conditions or pregnancy-related complications. Comprehensive interaction screening should be incorporated into individualized supplementation protocols to prevent interference with medication effectiveness or increased risk of adverse effects.
Quality control and standardization of testing methodologies become increasingly important as supplementation becomes more individualized and precise, with rigorous standards needed to ensure accuracy and reliability of biomarker assessments and genetic testing used to guide supplementation decisions.
Conclusion
The evolution toward precision nutrition approaches in pregnancy represents a fundamental shift from universal supplementation strategies to individualized interventions that recognize the remarkable heterogeneity in micronutrient requirements and metabolism among pregnant women. This transformation reflects growing understanding of the complex interactions between genetic factors, environmental influences, and physiological adaptations that determine optimal nutritional status during pregnancy and its impact on maternal and fetal health outcomes.
The implementation of precision nutrition requires integration of advanced diagnostic approaches, comprehensive risk assessment, and individualized supplementation strategies that address the unique characteristics and needs of each pregnant woman. This personalized approach offers unprecedented opportunities to optimize maternal micronutrient status while minimizing risks of both deficiency and toxicity that can affect pregnancy outcomes.
Future developments in precision nutrition will likely incorporate increasingly sophisticated technologies, including artificial intelligence, advanced biomarker assessment, and personalized supplement formulations, to provide more precise and effective nutritional interventions during pregnancy. The continued advancement of this field holds promise for significantly improving maternal and fetal health outcomes through optimized nutritional care tailored to individual requirements and characteristics.
Table 1: Critical Micronutrients and Precision Assessment Strategies
| Micronutrient | Standard Assessment | Precision Markers | Genetic Factors | Individualization Strategy |
| Iron | Hemoglobin, Ferritin | Hepcidin, sTfR, ZPP | HFE, TMPRSS6 variants | Genetic-guided dosing, functional markers |
| Folate | Serum folate, RBC folate | Homocysteine, MMA | MTHFR C677T, A1298C | Genotype-based dosing, metabolite monitoring |
| Vitamin D | 25(OH)D | 1,25(OH)2D, PTH | VDR, CYP variants | Genetic risk, seasonal adjustment |
| Vitamin B12 | Serum B12 | MMA, Homocysteine | TCN1, FUT2 variants | Metabolite-guided therapy |
| Iodine | Urinary iodine | Thyroglobulin, TSH | TPO, TG variants | Thyroid function integration |
| Zinc | Serum zinc | Alkaline phosphatase | ZIP4, ZnT variants | Functional enzyme activity |
Table 2: Special Population Considerations for Precision Nutrition
| Population | Unique Risk Factors | Modified Requirements | Assessment Considerations | Specialized Interventions |
| Adolescents | Growth demands, poor diet | Increased for most nutrients | Bone markers, growth velocity | Enhanced monitoring, education |
| Multiple pregnancies | Higher fetal demands | 1.5-2x standard requirements | More frequent assessment | Higher dose protocols |
| Vegetarians/Vegans | Limited animal nutrients | B12, iron, zinc, DHA | Bioavailability assessment | Specialized formulations |
| Ethnic minorities | Genetic variations | Population-specific needs | Cultural dietary patterns | Culturally appropriate approaches |
| Chronic diseases | Altered metabolism | Disease-specific modifications | Medication interactions | Coordinated care protocols |
Table 3: Emerging Technologies in Precision Nutrition
| Technology | Application | Current Status | Future Potential | Implementation Barriers |
| Nutrigenomics | Genetic-based recommendations | Research/Early adoption | Personalized protocols | Cost, interpretation complexity |
| Metabolomics | Functional status assessment | Research phase | Real-time monitoring | Technical complexity, standardization |
| AI/Machine Learning | Pattern recognition, prediction | Development phase | Automated recommendations | Data quality, validation needs |
| Point-of-care testing | Rapid deficiency detection | Limited availability | Widespread screening | Accuracy, cost considerations |
| Digital therapeutics | Monitoring, adherence | Early deployment | Integrated care platforms | User engagement, data security |
| Personalized supplements | Individual formulations | Limited availability | Precise dosing | Manufacturing, regulatory issues |
 pregno-world.com
pregno-world.com