Postpartum depression represents one of the most significant and prevalent complications of childbearing, affecting between ten and twenty percent of new mothers worldwide and creating profound implications that extend far beyond individual maternal suffering to encompass infant development, family functioning, and long-term public health outcomes. This complex condition emerges from the intersection of biological vulnerability, psychological adaptation, and social circumstances, requiring sophisticated understanding and multifaceted therapeutic approaches that address not only maternal symptoms but also the intricate dynamics of early parent-child relationships that form the foundation for lifelong emotional and cognitive development.
The recognition that postpartum depression affects not merely the mother but the entire family system has revolutionized approaches to diagnosis and treatment, moving beyond traditional models that focus solely on maternal symptomatology toward comprehensive interventions that simultaneously address maternal mental health, infant wellbeing, and the quality of early relational experiences. This evolution reflects growing awareness that the period immediately following childbirth represents a critical window for both maternal psychological adjustment and the establishment of secure attachment relationships that profoundly influence child development trajectories.
Contemporary understanding of postpartum depression emphasizes its multifactorial etiology, involving complex interactions between hormonal fluctuations, sleep deprivation, psychosocial stressors, and individual vulnerability factors that create a perfect storm for the development of mood disorders during the postpartum period. The condition manifests across a spectrum of severity, from mild adjustment difficulties to severe depression with psychotic features, requiring tailored interventions that match treatment intensity to symptom severity while considering the unique challenges faced by mothers caring for newborn infants.
Neurobiological Foundations and Pathophysiology
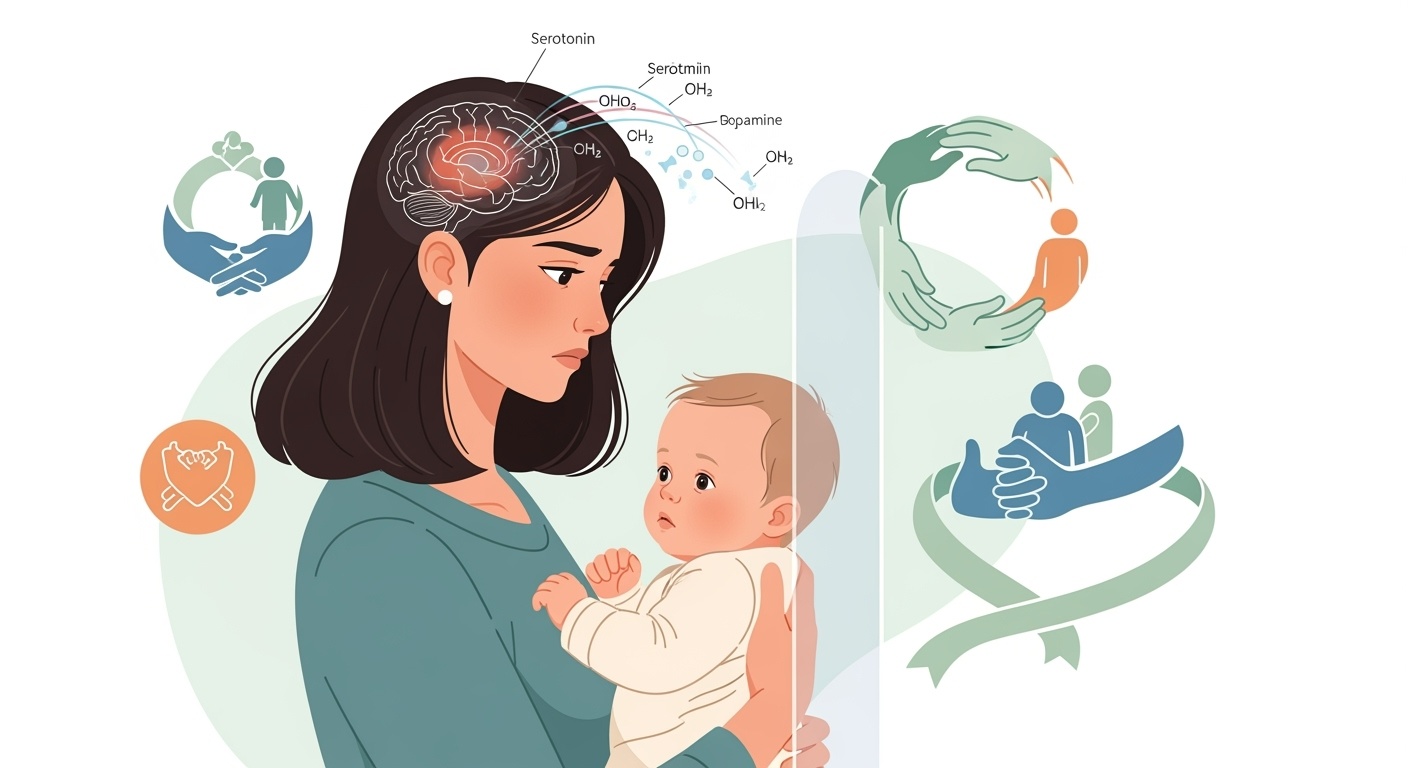
The neurobiological landscape of postpartum depression encompasses dramatic hormonal shifts, neurotransmitter dysregulation, and structural brain changes that occur during pregnancy and the immediate postpartum period, creating a complex biological substrate that predisposes vulnerable women to mood disorders. The precipitous decline in estrogen and progesterone levels following delivery represents one of the most significant hormonal changes experienced by the human body, with estrogen levels dropping to postmenopausal ranges within days of childbirth and remaining suppressed for weeks to months, particularly in breastfeeding women.
These hormonal fluctuations profoundly affect neurotransmitter systems implicated in mood regulation, particularly serotonin, dopamine, and gamma-aminobutyric acid pathways that govern emotional stability, reward processing, and anxiety responses. The interaction between reproductive hormones and neurotransmitter function creates a cascade of neurochemical changes that can destabilize mood regulation in susceptible individuals, with the severity and duration of these changes influenced by genetic factors, previous psychiatric history, and environmental stressors.
Neuroimaging studies have revealed significant structural and functional brain changes during pregnancy and the postpartum period, including alterations in gray matter volume in regions associated with social cognition, empathy, and anxiety processing. These changes, while adaptive in many cases and associated with enhanced maternal sensitivity and caregiving behaviors, may contribute to increased vulnerability to mood disorders in women with predisposing risk factors.
The hypothalamic-pituitary-adrenal axis undergoes significant alterations during pregnancy and the postpartum period, with prolonged elevation of cortisol levels during pregnancy followed by dysregulated stress responses in the weeks following delivery. This disruption of normal stress response systems can contribute to the development and maintenance of depressive symptoms while also affecting maternal sensitivity to infant cues and the quality of early caregiving interactions.
Inflammatory processes also play a crucial role in postpartum depression pathophysiology, with elevated levels of pro-inflammatory cytokines observed in many women with postpartum depression. These inflammatory markers may result from the stress of childbirth, sleep deprivation, or psychosocial stressors, creating a biological environment that promotes depressive symptoms while potentially interfering with normal bonding processes and maternal responsiveness.
Risk Factors and Vulnerability Assessment
The identification of risk factors for postpartum depression has evolved from simple demographic considerations to sophisticated understanding of the complex interplay between biological predisposition, psychological vulnerability, and social circumstances that combine to create individual risk profiles. Personal history of mood disorders represents one of the strongest predictors of postpartum depression, with women who have experienced previous episodes of major depression facing significantly elevated risks for developing postpartum mood disorders.
Previous episodes of postpartum depression carry particularly high predictive value, with recurrence rates approaching fifty to eighty percent in subsequent pregnancies, highlighting the importance of early identification and preventive interventions for women with positive histories. The timing and severity of previous episodes provide important prognostic information, with early-onset and severe previous episodes associated with increased likelihood of recurrence and more severe symptomatology.
Family history of mood disorders creates additional vulnerability through both genetic and environmental pathways, with women having first-degree relatives with depression or bipolar disorder facing elevated risks that appear to be mediated through both inherited biological susceptibilities and learned patterns of emotional regulation and stress response. The interaction between genetic vulnerability and environmental stressors follows complex patterns that vary among individuals and require careful assessment to guide preventive and therapeutic interventions.
Psychosocial risk factors encompass a broad range of circumstances that can overwhelm individual coping resources and contribute to the development of postpartum depression. Relationship difficulties, including marital conflict, domestic violence, or lack of partner support, create chronic stress that depletes psychological resources needed for healthy adaptation to motherhood. Financial strain, housing instability, and social isolation compound these stresses, creating cumulative burden that can precipitate mood disorders in vulnerable individuals.
Pregnancy and delivery complications add additional layers of risk through both biological and psychological pathways. Preterm delivery, pregnancy loss, neonatal intensive care unit admissions, and breastfeeding difficulties can create trauma responses and ongoing stress that contribute to the development of postpartum depression while simultaneously interfering with normal bonding processes and maternal confidence.
The transition to motherhood itself represents a profound life change that requires significant psychological adjustment, with factors such as maternal age, parity, and role adjustment influencing individual vulnerability to mood disorders. Adolescent mothers face particular challenges related to developmental tasks and social support, while older mothers may experience increased anxiety related to pregnancy risks and fertility concerns.
Cultural and social factors play increasingly recognized roles in postpartum depression risk, with cultural expectations about motherhood, stigma associated with mental health problems, and access to social support varying dramatically across different communities and contributing to disparities in both risk and treatment access. Immigration status, language barriers, and cultural conflicts around childrearing practices can create additional stressors that increase vulnerability to postpartum mood disorders.
Clinical Presentation and Diagnostic Considerations
The clinical presentation of postpartum depression encompasses a complex constellation of symptoms that extend beyond traditional depressive symptoms to include specific concerns related to motherhood, infant care, and family adjustment. While core depressive symptoms including persistent sadness, anhedonia, fatigue, and sleep disturbances form the foundation of the clinical picture, postpartum depression often presents with unique features that reflect the specific challenges and contexts of new motherhood.
Maternal anxiety represents a prominent and often predominant feature of postpartum depression, manifesting as excessive worry about infant health and safety, fear of harming the baby, and overwhelming concerns about maternal competence and adequacy. These anxiety symptoms often overshadow depressive symptoms in clinical presentation and may be the primary complaint that brings women to clinical attention, requiring careful assessment to identify underlying depressive processes.
Guilt and shame associated with perceived maternal inadequacy or negative feelings toward the infant represent particularly distressing symptoms that can prevent women from seeking help due to concerns about judgment or fear of having their children removed from their care. These feelings often center around societal expectations of maternal bliss and natural bonding, creating cognitive dissonance between expected and actual experiences that exacerbates depressive symptoms.
Sleep disturbances in postpartum depression extend beyond the normal sleep disruption associated with newborn care, with many women experiencing persistent insomnia even when opportunities for sleep are available. These sleep problems can create vicious cycles where sleep deprivation exacerbates depressive symptoms while depression interferes with the ability to obtain restorative sleep when possible.
Cognitive symptoms including difficulty concentrating, memory problems, and indecisiveness can significantly impact maternal functioning and contribute to feelings of incompetence and inadequacy. These cognitive changes may be particularly distressing for women who previously functioned at high levels professionally or academically, creating additional sources of stress and negative self-evaluation.
Physical symptoms including headaches, gastrointestinal problems, and chronic pain are common in postpartum depression and may be attributed to normal postpartum recovery, leading to delayed recognition and treatment. The overlap between normal postpartum physical symptoms and depression-related somatic complaints requires careful clinical assessment to avoid both over- and under-diagnosis.
The timing of symptom onset provides important diagnostic and prognostic information, with early-onset symptoms appearing within the first few weeks postpartum often associated with more severe courses and greater impact on mother-infant bonding. Late-onset postpartum depression, emerging months after delivery, may be associated with different risk factors and may require different therapeutic approaches.
Postpartum psychosis represents the most severe form of postpartum mood disorder, characterized by hallucinations, delusions, severe mood instability, and significant impairment in reality testing. This condition represents a psychiatric emergency requiring immediate intervention due to high risks of harm to both mother and infant, with delusions often centering around the infant and creating dangerous situations.
The differential diagnosis of postpartum depression includes consideration of normal postpartum adjustment, thyroid disorders, other medical conditions, substance use disorders, and pre-existing psychiatric conditions that may be exacerbated by pregnancy and delivery. Careful history-taking and appropriate laboratory studies help distinguish postpartum depression from other conditions that may present with similar symptoms.
Impact on Mother-Infant Bonding and Child Development
The relationship between postpartum depression and mother-infant bonding represents one of the most critical aspects of this condition, with research demonstrating profound and lasting effects on attachment formation, infant development, and family functioning that can persist for years beyond the acute depressive episode. Maternal depression interferes with the complex process of attachment formation through multiple pathways, including reduced maternal sensitivity, decreased responsiveness to infant cues, and impaired emotional availability during critical periods of early development.
Depressed mothers often exhibit flattened affect, reduced eye contact, and diminished vocal expressiveness during interactions with their infants, creating an emotional environment that lacks the rich affective exchanges necessary for healthy attachment formation. These alterations in maternal behavior occur at precisely the time when infants are developing fundamental expectations about relationships and learning to regulate their own emotional states through co-regulation with caregivers.
The quality of early mother-infant interactions profoundly influences infant brain development, particularly in regions associated with emotional regulation, stress response, and social cognition. Infants of depressed mothers show altered patterns of brain activity, including increased right frontal brain activity associated with withdrawal behaviors and negative emotionality, suggesting that maternal depression creates neurobiological changes in developing infants that may persist beyond the acute maternal illness.
Attachment security, which develops through consistent, sensitive, and responsive caregiving during the first year of life, is significantly compromised in dyads where mothers experience postpartum depression. Insecure attachment patterns, including anxious-ambivalent, avoidant, and disorganized attachment styles, are overrepresented among infants of depressed mothers, creating vulnerability to later emotional, behavioral, and social difficulties.
The timing of maternal depression appears to influence the nature and severity of infant effects, with depression during the first few months postpartum associated with more significant disruptions in attachment formation than later-onset depression. However, the duration and severity of maternal symptoms also play crucial roles, with chronic or recurrent depression creating cumulative effects that may be more detrimental than brief episodes of severe depression.
Infant regulatory capacities, including sleep patterns, feeding behaviors, and emotional self-regulation, are significantly affected by maternal depression through both direct effects on caregiving quality and indirect effects mediated through the quality of the mother-infant relationship. Infants of depressed mothers show increased rates of sleep difficulties, feeding problems, excessive crying, and difficulty with state regulation that can create additional stress for already overwhelmed mothers.
Cognitive and language development trajectories are also influenced by maternal depression, with research demonstrating effects on infant attention, learning, and early language development that appear to be mediated through the quality of maternal interactive behaviors and the richness of the linguistic environment provided by depressed mothers. These early effects on cognitive development can have cascading impacts on later academic achievement and intellectual functioning.
The intergenerational transmission of depression risk appears to begin during infancy, with children of mothers who experienced postpartum depression showing elevated rates of depression and anxiety disorders throughout childhood and adolescence. These effects appear to be mediated through both genetic mechanisms and environmental pathways, including the quality of early caregiving relationships and ongoing family functioning.
Comprehensive Assessment and Diagnostic Tools
The assessment of postpartum depression requires sophisticated evaluation approaches that go beyond traditional psychiatric screening to encompass the unique challenges and contexts of new motherhood, including evaluation of maternal functioning, infant wellbeing, and the quality of early relational experiences. The Edinburgh Postnatal Depression Scale represents the most widely used and extensively validated screening instrument for postpartum depression, providing a reliable and efficient method for identifying women at risk for or experiencing postpartum mood disorders.
The Edinburgh Postnatal Depression Scale consists of ten items that assess various aspects of mood, anxiety, and functioning during the postpartum period, with particular attention to feelings specific to motherhood including guilt, anxiety about the baby, and ability to cope with daily tasks. The scale can be administered at multiple time points throughout the postpartum period, providing valuable information about symptom trajectories and treatment response over time.
Clinical interviews remain the gold standard for diagnosing postpartum depression, requiring skilled clinicians who can elicit sensitive information about maternal experiences, thoughts about the infant, and functioning in various domains of life. These interviews should assess not only current symptoms but also personal and family psychiatric history, social support systems, relationship functioning, and specific stressors related to pregnancy, delivery, and early motherhood.
The assessment of suicidal ideation requires particular attention in postpartum depression, as traditional risk assessment approaches may not adequately capture the unique features of postpartum suicidal thinking, which may include thoughts of harming both oneself and the infant or fears of accidentally harming the baby through negligence or impaired judgment. Direct questioning about thoughts of harming oneself or the baby is essential, as many women will not volunteer this information due to shame or fear of consequences.
Evaluation of maternal functioning encompasses multiple domains including self-care, infant care, household management, and social functioning, with particular attention to the mother’s ability to respond appropriately to infant cues and provide safe, nurturing care. Observational assessments of mother-infant interactions can provide valuable information about the quality of early relationships and identify specific areas for intervention.
Assessment of infant wellbeing includes evaluation of growth and development, behavioral regulation, and signs of distress or developmental delays that may be associated with maternal depression. While direct causal relationships between maternal depression and infant problems can be difficult to establish, careful assessment of infant functioning provides important information for treatment planning and monitoring.
Social support assessment examines the availability and quality of support from partners, family members, friends, and community resources, as social support represents both a protective factor against postpartum depression and a crucial component of effective treatment approaches. The assessment should identify not only the quantity of available support but also the quality and appropriateness of support provided.
Cultural assessment considers the influence of cultural background, beliefs about motherhood and mental health, and potential barriers to treatment engagement that may affect both assessment accuracy and treatment planning. Cultural factors may influence symptom expression, help-seeking behaviors, and treatment preferences, requiring culturally sensitive approaches to both assessment and intervention.
Biological assessment may include thyroid function tests, complete blood count, and other laboratory studies to rule out medical conditions that may contribute to or mimic postpartum depression symptoms. Sleep assessment, nutritional evaluation, and substance use screening provide additional important information for comprehensive treatment planning.
Pharmacological Treatment Approaches
Pharmacological treatment of postpartum depression requires careful consideration of multiple factors including symptom severity, breastfeeding status, previous medication responses, and patient preferences, with treatment decisions guided by the principle of optimizing maternal mental health while minimizing potential risks to nursing infants. Selective serotonin reuptake inhibitors represent the first-line pharmacological treatment for postpartum depression, offering favorable risk-benefit profiles for both mother and infant when breastfeeding is desired.
Sertraline and paroxetine have emerged as preferred options for breastfeeding mothers due to their relatively low levels in breast milk and minimal infant exposure, with extensive research supporting their safety and efficacy in this population. These medications typically require several weeks to achieve full therapeutic effects, requiring patient education about expected timelines and the importance of medication adherence during the initial treatment period.
The decision to initiate pharmacological treatment involves careful risk-benefit analysis considering the severity of maternal symptoms, degree of functional impairment, and potential consequences of untreated depression for both mother and infant. Severe depression with significant functional impairment, suicidal ideation, or psychotic features generally warrant immediate pharmacological intervention regardless of breastfeeding status, as the risks of untreated severe depression typically outweigh potential medication risks.
Dosing strategies for postpartum depression often mirror those used for depression in other populations, though some women may require higher doses due to physiological changes associated with pregnancy and breastfeeding that can affect medication metabolism and distribution. Starting with lower doses and gradually titrating upward can help minimize side effects while allowing assessment of treatment response at each dose level.
Monitoring of medication effects requires attention to both therapeutic benefits and potential adverse effects, with particular focus on changes in mood, anxiety, sleep, and functioning that indicate treatment response. Side effect monitoring should include assessment of sedation, activation, gastrointestinal effects, and sexual side effects that may affect medication adherence and overall treatment satisfaction.
The duration of pharmacological treatment for postpartum depression typically extends for at least six to twelve months following symptom remission to prevent relapse, though individual factors including previous depression history, ongoing stressors, and patient preferences influence specific treatment duration decisions. Discontinuation of medication should be gradual and carefully monitored, with particular attention to signs of symptom recurrence.
Alternative pharmacological approaches may be considered for women who do not respond to first-line treatments or who experience significant side effects, including other classes of antidepressants, augmentation strategies, and specialized interventions such as ketamine or esketamine for treatment-resistant cases. These approaches require specialized expertise and careful monitoring due to limited safety data in postpartum populations.
The integration of pharmacological treatment with psychosocial interventions appears to enhance treatment outcomes beyond what can be achieved with either approach alone, supporting the use of combined treatment approaches for many women with postpartum depression. The timing and sequencing of different treatment modalities can be individualized based on symptom severity, patient preferences, and available resources.
Psychotherapeutic Interventions
Psychotherapeutic interventions for postpartum depression encompass a range of evidence-based approaches that address not only depressive symptoms but also the specific challenges and transitions associated with new motherhood, including role adjustment, identity changes, and relationship modifications that accompany the birth of a child. Cognitive-behavioral therapy has emerged as one of the most extensively studied and effective psychotherapeutic approaches for postpartum depression, offering structured interventions that target the cognitive distortions and behavioral patterns that maintain depressive symptoms.
Cognitive-behavioral therapy for postpartum depression incorporates standard CBT techniques while addressing specific themes relevant to new mothers, including unrealistic expectations about motherhood, perfectionist thinking patterns, and catastrophic interpretations of normal infant behaviors or maternal experiences. The therapy helps women identify and challenge negative thought patterns while developing more balanced and realistic perspectives about motherhood and their own capabilities as mothers.
Behavioral activation represents a crucial component of CBT for postpartum depression, helping women gradually resume activities that provide pleasure and mastery while managing the practical challenges of caring for a newborn. This approach is particularly valuable for women who have become socially isolated or who have abandoned self-care activities due to depression or overwhelming caregiving demands.
Interpersonal therapy has demonstrated significant efficacy for postpartum depression, focusing on the relationship difficulties and role transitions that often contribute to or result from postpartum mood disorders. This approach helps women navigate the complex changes in relationships with partners, family members, and friends that often accompany the transition to motherhood while addressing grief related to losses of previous identity and lifestyle.
The role transition focus of interpersonal therapy is particularly relevant for postpartum depression, as becoming a mother represents one of the most significant life transitions individuals experience, requiring fundamental changes in identity, priorities, and daily functioning. The therapy helps women develop realistic expectations about this transition while building skills for managing the challenges and conflicts that arise.
Psychodynamic therapy approaches for postpartum depression explore the unconscious conflicts and early relationship patterns that may contribute to difficulties with maternal identity formation and bonding with the infant. This approach can be particularly valuable for women with histories of trauma or difficult relationships with their own mothers that may interfere with their ability to develop confident, nurturing relationships with their infants.
Group therapy formats offer unique advantages for postpartum depression treatment, providing opportunities for social support, normalization of experiences, and learning from other mothers facing similar challenges. Support groups, psychoeducational groups, and structured therapy groups all offer different benefits and can be tailored to meet the specific needs and preferences of different women.
The timing and format of psychotherapy delivery requires careful consideration of the practical challenges faced by new mothers, including childcare needs, transportation difficulties, and unpredictable infant schedules. Flexible scheduling, home-based services, and telehealth options can improve access to psychotherapeutic interventions for women who might otherwise be unable to participate in traditional office-based therapy.
Dyadic and Family-Centered Interventions
Dyadic interventions that simultaneously address maternal depression and mother-infant relationship quality represent innovative treatment approaches that recognize the interconnected nature of maternal mental health and infant wellbeing, offering the potential to improve outcomes for both members of the mother-infant dyad through targeted interventions that enhance relational functioning. Mother-infant psychotherapy integrates principles from psychodynamic therapy, attachment theory, and developmental psychology to address both maternal psychological symptoms and the quality of early relational experiences.
The theoretical foundation of mother-infant psychotherapy rests on the understanding that infant mental health and development are inextricably linked to the quality of caregiving relationships, and that addressing maternal depression without attention to relational functioning may not fully optimize outcomes for either mother or infant. These interventions typically involve joint sessions with mother and infant, allowing therapists to observe interactions directly and provide real-time feedback and guidance.
Watch, Wait, and Wonder represents a specific dyadic intervention that encourages mothers to follow their infant’s lead during play sessions while therapists help mothers understand and respond to infant cues more effectively. This approach helps depressed mothers, who may be less attuned to infant signals, develop greater sensitivity and responsiveness while building confidence in their maternal capabilities.
Toddler-parent psychotherapy extends dyadic approaches to older children who may have been affected by maternal depression during infancy, addressing the ongoing effects of early relational difficulties while helping mothers and children develop healthier interaction patterns. This approach is particularly valuable for families where maternal depression has been chronic or recurrent, creating ongoing challenges in parent-child relationships.
Circle of Security interventions focus specifically on attachment relationships, helping mothers understand their infant’s attachment needs and develop more secure caregiving behaviors through education about attachment theory combined with video review of parent-child interactions. This approach can be particularly effective for mothers whose own attachment histories may interfere with their ability to provide secure caregiving.
Video feedback interventions use recordings of mother-infant interactions to help mothers recognize positive aspects of their caregiving while identifying areas for improvement, providing concrete feedback that can enhance maternal sensitivity and confidence. These approaches are particularly valuable for depressed mothers who may have difficulty recognizing their own strengths and positive contributions to their infant’s development.
Family therapy approaches recognize that postpartum depression affects entire family systems, including partners, other children, and extended family members who may be struggling to understand and respond to maternal depression. These interventions address communication patterns, role adjustments, and support systems that can either contribute to or help resolve postpartum depression.
Partner-focused interventions recognize the crucial role that intimate partners play in both the development and resolution of postpartum depression, offering education about postpartum depression, communication skills training, and support for partners who may be struggling with their own adjustment to parenthood and their partner’s depression.
| Intervention Type | Primary Focus | Target Population | Duration | Key Outcomes |
| Mother-Infant Psychotherapy | Maternal symptoms and dyadic relationship | Mother-infant dyads | 12-20 sessions | Improved maternal depression, enhanced infant attachment security |
| Watch, Wait, Wonder | Maternal sensitivity and infant-led interactions | Mothers with interaction difficulties | 10-14 sessions | Increased maternal responsiveness, improved infant emotional regulation |
| Circle of Security | Attachment understanding and secure caregiving | At-risk mother-infant dyads | 8-week groups | Enhanced attachment security, reduced maternal anxiety |
| Video Feedback Therapy | Interaction quality and maternal confidence | Mothers with low sensitivity | 6-10 sessions | Improved interaction quality, increased maternal self-efficacy |
Home-Based and Community Interventions
Home-based interventions for postpartum depression address multiple barriers to treatment access while providing services in the natural environment where mother-infant interactions occur, offering unique opportunities for assessment and intervention that cannot be replicated in traditional office settings. These approaches recognize that many women with postpartum depression face significant practical barriers to accessing traditional mental health services, including transportation difficulties, childcare challenges, and social isolation that may prevent engagement with clinic-based treatments.
Nurse home visiting programs represent one of the most extensively studied home-based interventions for postpartum depression, combining mental health screening and intervention with traditional postpartum care and infant health monitoring. These programs typically involve regular visits by trained nurses who can provide depression screening, basic counseling interventions, referral to specialized mental health services, and ongoing support throughout the postpartum period.
The integration of mental health services with routine postpartum care helps normalize mental health concerns while ensuring that depression screening and intervention become routine components of postpartum healthcare rather than specialized services that require separate referrals. This integration can significantly improve identification and treatment rates for postpartum depression while reducing stigma associated with mental health service utilization.
Peer support interventions utilize trained mothers who have previously experienced postpartum depression to provide support, education, and advocacy for women currently experiencing depression, offering unique perspectives and credibility that may not be available through professional interventions alone. These peer supporters can provide practical advice about managing depression while caring for infants, share strategies that have been effective in their own recovery, and offer hope for improvement based on their personal experiences.
Community health worker models adapt home-based interventions for diverse cultural and linguistic communities, training individuals from specific communities to provide culturally appropriate mental health support and navigation services. These approaches can be particularly effective for immigrant communities, communities of color, and other populations that may face barriers to accessing traditional mental health services.
Telephone and digital health interventions extend the reach of home-based services by providing support and intervention through remote technologies, offering particular advantages for women in rural areas or those with severe mobility limitations. These approaches can provide crisis support, ongoing therapy sessions, educational resources, and peer connections that might otherwise be unavailable.
Infant massage interventions teach mothers techniques for providing therapeutic touch to their infants while providing opportunities for positive mother-infant interactions that can enhance bonding and maternal confidence. These interventions can be particularly valuable for mothers who are struggling with feelings of disconnection from their infants or who lack confidence in their caregiving abilities.
Comprehensive home-based programs combine multiple intervention components including mental health treatment, parenting education, social support, and connections to community resources, offering intensive support for women with complex needs or multiple risk factors. These programs recognize that postpartum depression often occurs in the context of multiple stressors and challenges that require comprehensive rather than narrow intervention approaches.
The effectiveness of home-based interventions appears to be enhanced by their ability to address both individual and environmental factors that contribute to postpartum depression, including social isolation, lack of practical support, and disconnection from community resources. By providing services in women’s homes, these interventions can directly address environmental stressors while building support systems within women’s natural communities.
Cultural Considerations and Diverse Populations
Cultural factors profoundly influence the experience, expression, and treatment of postpartum depression, requiring culturally responsive approaches that acknowledge the diverse ways in which different communities understand motherhood, mental health, and help-seeking behaviors. Cultural beliefs about the postpartum period vary dramatically across different ethnic and cultural groups, with some cultures emphasizing extended rest and family support during the postpartum period while others expect rapid return to normal functioning and independence.
The expression of postpartum depression symptoms may vary across cultural groups, with some cultures emphasizing somatic complaints rather than emotional symptoms, while others may interpret depression symptoms as spiritual or moral problems rather than medical conditions. These variations in symptom expression require culturally informed assessment approaches that can identify depression across different cultural contexts without imposing Western-centric diagnostic frameworks.
Stigma associated with mental illness varies significantly across different cultural communities, with some groups viewing mental health problems as shameful or reflecting poorly on family honor, while others may be more accepting of mental health difficulties as medical conditions requiring treatment. Understanding and addressing cultural stigma is crucial for engaging women from diverse backgrounds in treatment while avoiding approaches that may inadvertently increase shame or resistance to help-seeking.
Traditional postpartum practices in many cultures include specific dietary restrictions, activity limitations, and family support systems that may either protect against or contribute to postpartum depression depending on individual circumstances and the degree to which traditional practices are maintained in modern contexts. Understanding these traditional practices is important for developing culturally appropriate treatment recommendations that work within rather than against cultural expectations.
Language barriers can significantly impair both assessment and treatment of postpartum depression, requiring availability of interpretation services, translated materials, and bilingual mental health providers who can provide culturally and linguistically appropriate care. The nuances of mental health terminology may not translate directly across languages, requiring careful attention to cultural concepts of distress and healing.
Immigration status and acculturation stress create additional risk factors for postpartum depression among immigrant women, who may be navigating new healthcare systems, language barriers, and separation from traditional support systems while adjusting to motherhood. These women may also face unique stressors related to documentation status, employment restrictions, and discrimination that compound the challenges of postpartum adjustment.
Religious and spiritual beliefs play important roles in many women’s understanding of postpartum depression and their willingness to engage in different types of treatment, requiring assessment of spiritual resources and potential integration of religious or spiritual elements into treatment approaches when appropriate and desired by clients.
Socioeconomic factors intersect with cultural factors to create unique challenges for women from diverse backgrounds, with poverty, housing instability, and limited access to healthcare creating additional barriers to both prevention and treatment of postpartum depression. Culturally responsive interventions must address these structural barriers while respecting cultural values and preferences.
Prevention Strategies and Early Intervention
Prevention of postpartum depression represents a crucial public health opportunity that requires identification of at-risk women during pregnancy combined with targeted interventions designed to reduce risk factors and enhance protective factors before depression develops. Universal screening during pregnancy and the postpartum period forms the foundation of prevention efforts, identifying women with risk factors who might benefit from enhanced monitoring and early intervention services.
Prenatal education about postpartum depression can help normalize the condition while preparing women and their families to recognize early warning signs and seek help promptly when needed. This education should address myths and misconceptions about postpartum depression while providing accurate information about symptoms, risk factors, and available treatments that can encourage help-seeking behavior.
Enhanced prenatal care for high-risk women may include more frequent visits, additional screening, and connections to mental health services before delivery, providing opportunities to address risk factors and build therapeutic relationships that can facilitate rapid intervention if depression develops. This enhanced care should be integrated with routine prenatal services to avoid stigmatization while ensuring comprehensive support.
Partner and family education represents an important component of prevention efforts, as intimate partners and family members are often the first to recognize changes in maternal mood and functioning and may play crucial roles in encouraging help-seeking and providing support during treatment. Education should include information about how to provide effective support while avoiding common mistakes that may inadvertently worsen depression.
Psychosocial interventions during pregnancy for high-risk women have shown promise for preventing postpartum depression, particularly approaches that address relationship difficulties, build coping skills, and enhance social support systems before delivery. These interventions may be particularly valuable for women with histories of depression or significant psychosocial stressors.
Immediate postpartum interventions focus on the critical first few weeks following delivery when risk for depression onset is highest, providing enhanced support, monitoring, and rapid access to treatment services when early symptoms are identified. These interventions may include home visits, telephone support, and expedited access to mental health services that can prevent progression from mild symptoms to major depression.
Sleep enhancement interventions recognize the crucial role that sleep deprivation plays in postpartum depression development, providing education and support for optimizing sleep despite newborn care demands. These interventions may include guidance about sleep hygiene, strategies for maximizing sleep opportunities, and family support for nighttime infant care responsibilities.
Breastfeeding support interventions address the relationship between breastfeeding difficulties and postpartum depression risk, providing early and intensive lactation support that can prevent the disappointment and stress associated with breastfeeding challenges that may contribute to depression development.
Social support interventions work to enhance existing support systems while building new connections for women who may be socially isolated, recognizing that strong social support represents one of the most important protective factors against postpartum depression. These interventions may include peer support programs, new mother groups, and family support services.
| Prevention Level | Target Population | Intervention Type | Timing | Expected Outcomes |
| Universal | All pregnant women | Education and screening | Prenatal and postpartum | Increased awareness, early identification |
| Selective | High-risk women | Enhanced support and monitoring | Pregnancy through early postpartum | Reduced incidence in at-risk population |
| Indicated | Women with early symptoms | Rapid intervention services | Early postpartum period | Prevention of progression to major depression |
Long-term Outcomes and Follow-up Care
Long-term outcomes following postpartum depression vary considerably depending on factors including symptom severity, treatment adequacy, ongoing stressors, and individual resilience factors, with research indicating that while many women recover completely from postpartum depression, others may experience chronic or recurrent mood difficulties that require ongoing management and support. The trajectory of recovery is influenced by multiple factors including the timeliness and appropriateness of treatment, the presence of ongoing stressors, and individual factors such as personality characteristics and coping skills.
Complete recovery from postpartum depression is possible for the majority of women who receive appropriate treatment, with symptoms typically improving significantly within three to six months of treatment initiation when effective interventions are provided. However, the definition of recovery extends beyond symptom resolution to include restoration of maternal functioning, improvement in mother-infant relationships, and return to previous levels of social and occupational functioning.
Relapse and recurrence risks remain elevated for women who have experienced postpartum depression, with studies indicating that approximately twenty-five to fifty percent of women may experience subsequent episodes of depression during future pregnancies or at other times in their lives. These risks highlight the importance of ongoing monitoring and maintenance treatment strategies that can prevent or minimize future episodes.
The long-term effects of postpartum depression on children depend heavily on factors including the duration and severity of maternal depression, the quality of treatment received, and the presence of ongoing family support and stability.
 pregno-world.com
pregno-world.com